Give your product, strategy and actuarial teams the comprehensive competitive intelligence they need to optimize plans for profitability and enrollment.
Identify what changed in competitor benefits within 48 hours of CMS release
Detect AEP disruption patterns and respond before enrollment shifts
Extract benefit language directly from EOCs to spot real competitor differences
Analyze Part D formularies and cost-sharing strategies across every competitor
“We pulled comprehensive benefit analysis across 25 markets in 2 days instead of 2 weeks. ProductIntel eliminated the manual EOC hunting that consumed our entire Q4.”
— Director of Product Strategy, Top 10 Health Plan
From AEP response to annual planning, ProductIntel delivers the competitive intelligence that drives confident product decisions
AEP Response & Market Defense
Detect competitive disruption as it happens. Track service area changes and member impact. Model rapid response strategies before enrollment shifts.
Pre-Bid Intelligence
Compare current designs against every competitor. Identify over-investment and competitive gaps. Export color-coded comparisons for Actuaries and finance.
Pharmacy & Formulary Strategy
Pressure-test Part D competitiveness across tiers and top drugs. Identify formulary gaps to exploit or weaknesses to address.
Portfolio Optimization
Understand which benefit designs drove growth post-AEP. Inform next year's strategy using intelligence from 5,000+ plans, 3,300+ counties, and more than 80 organizations.
Built for Cross-Functional Teams
Product leaders design competitive packages. Actuaries leverage True Plan Value (TPV) benchmarking during bid season. Strategy teams track disruption patterns. Executives make portfolio decisions backed by comprehensive intelligence.
ProductIntel structures competitive intelligence into actionable capabilities that accelerate your bid strategy.
Side-by-side comparisons across hundreds of benefit fields—dental codes, vision allowances, supplemental coverage. Color-coded deltas highlight changes. One-click Excel exports for Actuarial reviews.
Side-by-side comparisons across hundreds of benefit fields—dental codes, vision allowances, supplemental coverage. Color-coded deltas highlight changes. One-click Excel exports for Actuarial reviews.
Side-by-side comparisons across hundreds of benefit fields—dental codes, vision allowances, supplemental coverage. Color-coded deltas highlight changes. One-click Excel exports for Actuarial reviews.
5,000+ EOC Documents
Comparison analysis enabled with one-click download
200GB+ Data Processed
Harmonizes benefit and plan data annually across all sources
800+ Dental Code Analyses
Across 4,000+ bids covering national and major regional payers
3,000+ Counties
Complete competitive coverage across all markets
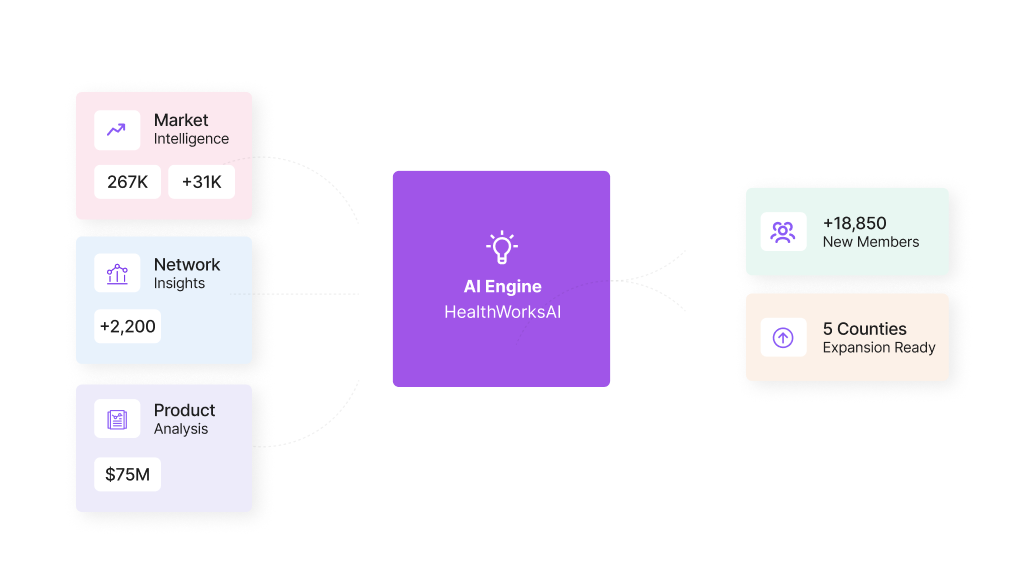
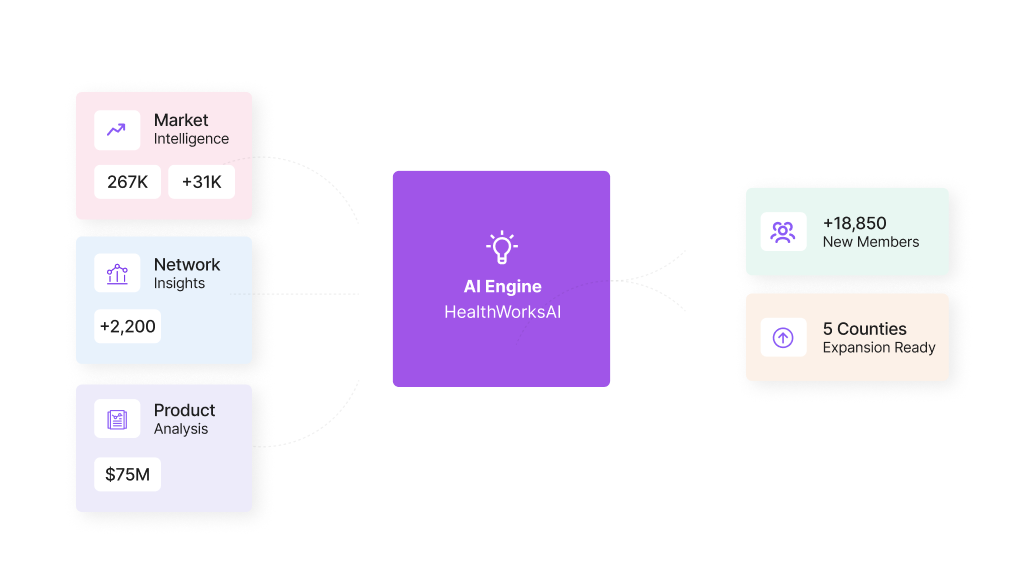
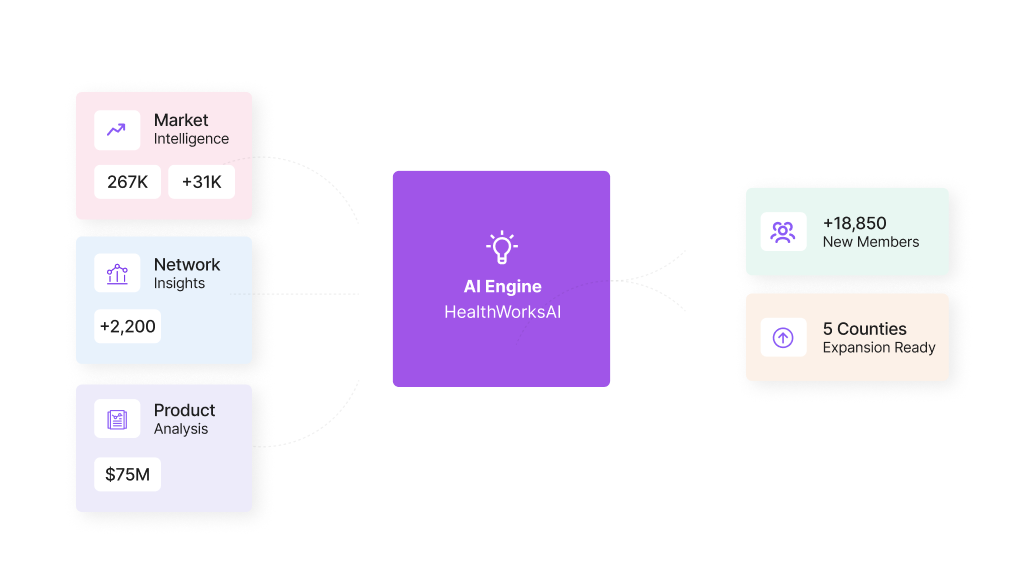
ProductIntel shows you what changed and how you compare. Pair it with our other products to complete your competitive advantage.
Within 48 hours of CMS releases, all plan and benefit data is parsed, structured, and ready for side-by-side comparisons. This includes the landscape files released in September and the October annual releases and monthly updates throughout the year.
ProductIntel combines PBP files, EOC documents, landscape data, crosswalk files, monthly enrollment data and HWAI proprietary data into a single structured platform. This comprehensive and structured data approach reveals benefit details that individual data sources miss and saves huge amounts of time.
TPV uses predictive analytics to assign dollar values to plan designs, quantifying how likely members are to prefer one plan over another. It incorporates medical benefits, supplemental coverage, and Part D protection into a single competitive metric—most valuable during bid season (January-July) for validating assumptions before submission.
Yes. Color-coded benefit comparisons export to Excel with one click, preserving the on-screen view exactly as you see it. This eliminates manual spreadsheet builds and accelerates stakeholder review cycles. Combine it with internal data sources to deepen your insights.
Product leaders designing competitive benefit packages, actuaries validating bid assumptions, pharmacy strategists pressure-testing formulary decisions, market intelligence teams tracking competitive moves, and executive leadership making portfolio decisions.
ProductIntel tracks material plan design changes post-release—supplemental benefits added, cost-sharing reduced, formulary enhancements, service area expansions or reductions. You see exactly what changed, which competitors moved, and how many members are impacted.